by Ahimsa Porter Sumchai MD, PD (Postdoctoral Fellow)
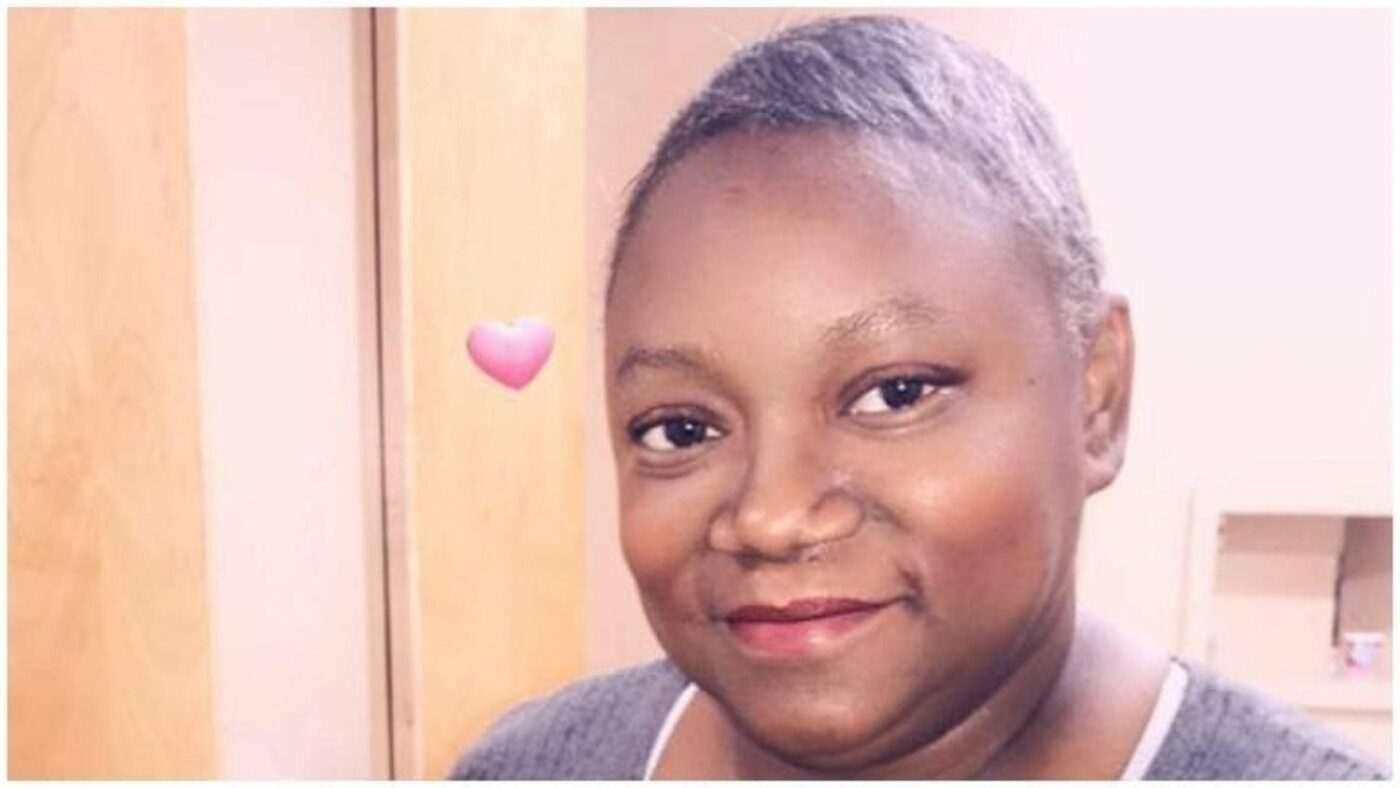
An enormous outpouring of empathy has been generated by the fully preventable, untimely and iconic death of Dr. Susan Moore. Her death ignited a “lightning rod” of debate about well known and well documented health disparities and poor disease outcomes seen in African Americans and other minority groups.
In COVID-19 it is termed BAME, the disproportionately high death rate seen in Black, Asian and other minority and ethnic groups. This population cohort is 27 percent overrepresented in COVID-19 deaths. Additionally, according to The Guardian, 63 percent of the first 106 health and social care staff known to have died from the virus were Black or Asian, as recorded by the Health Service Journal.
I fully agree with sympathizers who recognize this to be a nationally amplified example of the discourteous, demeaning and dismissive treatment women of color in particular often report in interactions with healthcare providers … particularly white men!
As a practicing physician and researcher, I promise to write a book one day about the spectrum of encounters I have had – as an expert patient – with overworked and callous care providers during my moments of deepest need. What disturbs me most about the circumstances surrounding Dr. Moore’s preventable death is not the medical racism … it is the medical negligence and malpractice!
It is not the “technical competency” of the care she deserved, yet did not receive after demanding it and demonstrating knowledge of medical standards of care. It is the lack of professional camaraderie and lack of professional courtesy she received from medical colleagues that is most egregious.
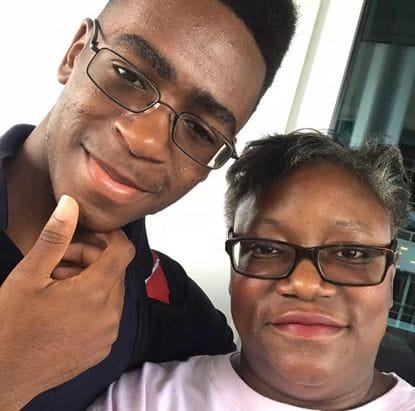
Dr. Susan Moore died of COVID-19 two weeks after documenting the substandard care she had received during an emergency visit she was discharged from, despite presenting with multiple signs, symptoms and risk factors for severe rapidly evolving COVID-19 pulmonary disease. Dr. Moore is a physician who cared for a 19-year-old son and parents who suffer from dementia.
I am inspired by the excellent professional analyses that have been generated that offer a base of fact upon which it can be concluded that Dr. Moore’s preventable death was contributed to by medical malpractice, neglect and substandard care. Dr. Omolara Uwemedimo offers factually based medical information about the actual care Dr. Moore received in a televised interview.
Dr. Moore presented with multiple high risk symptoms and co-morbidities known to worsen COVID-19 outcomes. She was breathing rapidly and complained of shortness of breath. She reported severe neck pain and a fever which, in my professional opinion – as a Stanford Fellowship-trained Board Certified Emergency Physician – means rule out meningitis!
Dr. Moore did not die from medical racism. She died from medical malpractice, neglect and lack of professional courtesy following abrupt discharge from an emergency department after presenting with multiple risk factors, comorbidities and symptoms of severe, rapidly evolving COVID-19 lung disease.
As a practicing physician, Dr. Moore knew a chest xray might not reveal early findings of COVID -19 lung disease and insisted on a study called a high resolution CT scan.
What is clear is that Dr. Moore’s signs, symptoms, risk factors and co-morbidities warranted hospitalization!
The hospital released a statement that appears to take the position that the level of care and technical competence of the visit was not an issue while acknowledging lapses in courtesy they plan to address with “trainings” while conducting a full review of the case.
It has been defensively argued that this lapse in professional courtesy by an attending physician toward a peer and physician colleague might have been the result of the overburdened, overcrowded, emotionally draining emergency care systems COVID-19 has spawned. That would, in fact, be a driving factor were it not for the archive of medical literature that substantiates racial bias in pain assessment and treatment recommendations instantaneously available on any internet search engine:
I had an episode in 2006 after sustaining a work related injury to my spine at multiple levels. I experienced new onset sciatica that radiated like a lighting bolt down my leg. In unrelenting pain, I sought care at UCSF Moffitt Emergency Department. There were memories triggered of rotating through this ER in 1982 as a resident in the Department of Neurological Surgery under founding chair, Charles B. Wilson.
After being escorted to an exam room and experiencing extreme pain just getting undressed, a young white male resident “popped” in unannounced. He did not introduce himself but wore a UCSF photo ID identifying him as a second year medical resident.
I explained to him that I was experiencing “new onset neuropathic pain in my leg” and believed I had herniated a lumbar disc. I wanted to see if I could get an injection of the non-narcotic Toradol for pain and be scheduled for an MRI scan. He looked at me in awe clearly questioning how I came to understand those medical terms.
Without addressing the obvious question on his face, I revealed I had trained in neurological surgery at UCSF and rotated as a resident through the same ER he was training in. The spread of disbelief on his face animated his explosive exclamation: “No, you didn’t!”
I couldn’t believe his disbelief! I knew the best way to advance my care was to request to be seen by his Chief Resident. Sensing an impending complaint and embarrassing incident, within 15 minutes the senior resident entered my exam room and I was responded to in a more respectful manner.
My point is that Dr. Moore did not die from medical racism. She died from medical malpractice, neglect and lack of professional courtesy following abrupt discharge from an emergency department after presenting with multiple risk factors, comorbidities and symptoms of severe, rapidly evolving COVID-19 lung disease. Additionally, she complained of severe neck pain that warranted a meningitis work-up. Dr. Moore requested standard of care treatment with the antiviral Remdesivir. She received two of the 10 recommended doses … and two weeks later died.
Dr. Moore is survived by a 19-year-old son and parents she cared for who both have dementia. A GoFundMe campaign will assist her family: https://www.gofundme.com/f/dr-susan-moores-family-assistance.
SF Bay View Health and Environmental Science Editor Ahimsa Porter Sumchai, MD, PD, founder and principal investigator for the Hunters Point Community Biomonitoring Program, founding chair of the Hunters Point Naval Shipyard Restoration Advisory Board’s Radiological Subcommittee and contributor to the 2005 Draft Historical Radiological Assessment, can be reached at AhimsaPorterSumchaiMD@Comcast.net. Dr. Sumchai is medical director of Golden State MD Health & Wellness, a UCSF and Stanford trained author and researcher, and a member of the UCSF Medical Alumni Association Board of Directors.