by Barry Hermanson
Oct. 15 through Dec. 7 is the annual Open Enrollment Period when Medicare beneficiaries can change their health or drug coverage for the coming year.
“You can join, switch or drop a Medicare Advantage Plan or Medicare drug plan, or switch to Original Medicare.” Also, “If you’re in a Medicare Advantage Plan, you can change to a different Medicare Advantage Plan or switch to Original Medicare (and join a separate Medicare drug plan)” one time from Jan. 1 through March 31, according to the official U.S. government Medicare handbook.
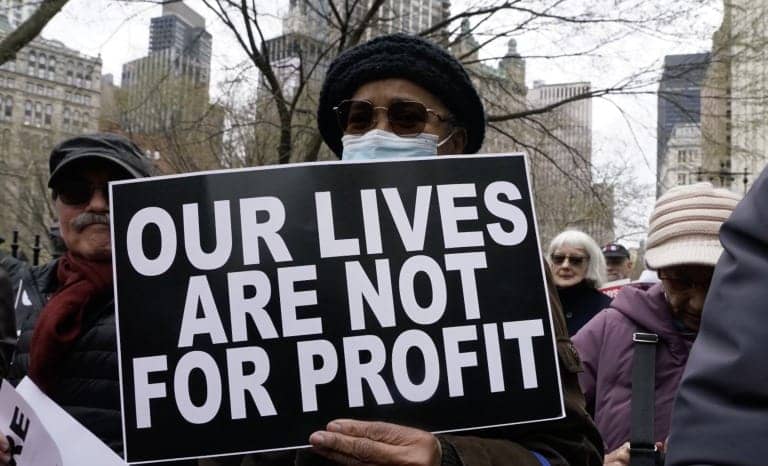
When you choose a Medicare Advantage Plan instead of receiving traditional Medicare, the government pays the provider “a set rate per person, per year (around $12,000 in 2019, not including Part D-related expenses) under what is called a ‘risk-based’ contract. That means that each plan agrees to assume the full risk of providing all care for that inclusive amount,” The Commonwealth Fund explains.
In an Aug. 25, 2022, letter to the administrator of the Centers for Medicare & Medicaid Services, Susan Rogers, M.D., president of Physicians for a National Health Program, wrote:
“MA plans use marketing tactics (including variations in coverage and contracting with employers to directly enroll newly Medicare eligible retirees) that attract healthier beneficiaries, and they employ multiple tactics to deny care to the sick, including narrow networks, formulary restrictions, and prior authorization. Sicker enrollees, such as in the last year of life, who have been frustrated by denial or delay of services tend to disenroll and return to the traditional Medicare program. The effect of both marketing tactics (‘cherry-picking’) and disenrollment of sicker beneficiaries (‘lemon-dropping’) is to create for Medicare Advantage plans a healthier and less costly than average risk pool. …
“Medicare Advantage plans have achieved profitability largely by gaming their risk pools, up-coding, and blunt restrictions on care including issuing millions of inappropriate denials for care that met Medicare coverage rules, and minimally if at all by improving care. Typical administrative costs for Medicare Advantage plans, including profits, have been in the 15-20% range, compared to around 2% for Traditional Medicare prior to the Affordable Care Act.”
In the eight years I have been enrolled in Medicare, my health expenses have been minimal. Except for one year, I have been enrolled in traditional Medicare. Because CMS (Centers for Medicare & Medicaid Services), over the last seven years, did not pay out $12,000 or more per year to a Medicare Advantage provider to cover the “risk” of handling my healthcare, Medicare saved more than $80,000.
When I became eligible for Medicare on my 65th birthday, I received multiple advertisements in the mail each week from Medicare Advantage providers before and during the Open Enrollment Period. This was repeated every year until now. This year, I received only two, a dramatic reduction from prior years. It must be because I’m older. I’m not as good a candidate to generate profits.
From an Overpayment Report recently released by Physicians for a National Health Program:
“By our estimate, and based on 2022 spending, Medicare Advantage overcharges taxpayers by a minimum of 22% or $88 billion per year, and potentially by up to 35% or $140 billion.”
“To put the sheer magnitude of overcharging in MA in perspective, a CBO analysis of a 2019 bill proposing to add dental, hearing and vision benefits to Medicare and Medicaid estimated that in the most expensive year of its implementation, these benefits would cost a combined $84 billion.”
A PNHP policy primer has this information:
“Medicare Advantage has grown substantially since its establishment in 2003, and now enrolls more than half of all Medicare beneficiaries. Insurance industry greed means that MA costs taxpayers more money while providing less care to patients, and the program is rife with accusations of fraud and bad behavior. There are many barriers to care for beneficiaries in MA plans, including narrow networks, prior authorization denials, and stringent limits on spending and coverage. Medicare for All would solve all of these issues, and is the only true solution to the problems our health care system faces.”
Dr. Rogers concludes her letter to the Centers for Medicare & Medicaid Services (CMS) with these words:
“It would be far more cost-effective for CMS to improve traditional Medicare by capping out-of-pocket costs and adding improved benefits within the Medicare fee-for-service system than to try to indirectly offer these improvements through private plans that require much higher overhead and introduce profiteers and perverse incentives into Medicare, enabling corporate fraud and abuse, raising cost to the Medicare Trust Fund, and worsening disparities in care.
“These problems are not correctable within the competitive insurance business model, and the Medicare Advantage program should be terminated.”
The Medicare Advantage mailers in your mailbox may look appealing and may provide some short-term benefit. Instead, beware: They are a disadvantage that endangers the solvency of the entire Medicare program.
Barry Hermanson is a member of the San Francisco Green Party and a former small business owner. Contact him at Barry@Hermansons.com or 415-255-9494.